Abstract
Venous thromboembolism (VTE) is a serious and common complication among cancer patients, both perioperatively and during hospitalization. The role of biomarkers in VTE prediction in this context is not well understood. The objective of this study was to summarize existing literature to identify candidate biomarkers capable of predicting the risk of VTE in perioperative and hospitalized cancer patients.
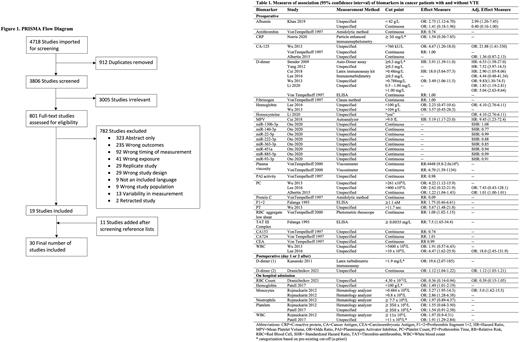
We searched Medline, EMBASE and Cochrane Central databases and references lists of included studies from inception until August 25th 2021. We included observational and interventional studies comprising of adult cancer patients who had blood biomarker measurements completed either at time of admission or during perioperative period. We only included studies reporting biomarker measurements prior to VTE events. Two reviewers screened the abstracts and full-texts independently and any disagreements were solved via consensus. We used the QUIPS risk of bias tool to assess study quality and risk of bias. This systematic review represents a substudy of a protocol registered in the Open Science Framework (https://osf.io/gqukw/links).
A total of 4718 studies were screened for eligibility (Figure 1). Thirty studies involving 61 biomarkers in 12896 patients with different cancer types and undergoing different procedures were included. The most frequent investigated biomarkers were d-dimer, fibrinogen, hemoglobin, platelet count and leukocyte counts. There was a significant difference in preoperative and early postoperative d-dimer levels between cancer patients with VTE and without VTE in three out of seven studies [mean (+/- standard deviation (SD)): VTE 2.31mg/L (0.56) versus non-VTE 0.71mg/L (0.07), p=0.002; VTE 3.3mg/L (1.7) versus non-VTE 2.7mg/L (3.5), p=0.021; VTE 1.2mg/L (1.8) versus non-VTE 0.5mg/L (0.2), p<0.001] and two out of two studies [mean (+/-SD): VTE 2.6 (2.8) versus non-VTE 1.2 (1.3), p=0.001; VTE 1.9 (0.8) versus non-VTE 0.9 (0.1), p=0.0009], respectively. Preoperative activated partial thromboplastin time, endogenous thrombin potential, hemoglobin, mean platelet volume, myeloperoxidase, plasma viscosity, plasmin inhibitor-plasmin complex, platelet count, red blood cell aggregation, soluble fibrin and, thrombin-antithrombin complex levels as well as monocyte count on admission were also significantly different between cancer patients with and without VTE in at least one study for each biomarker. The unadjusted and adjusted effect measures were included in Table 1. Adjustment for confounders differed in each study. The odds ratios (OR) and hazard ratios (HR) of VTE were increased for higher preoperative or early postoperative d-dimer levels and were statistically significant across multiple studies [preoperative OR (95% Confidence Interval (CI)): 3.49 (1.06-11.49); preoperative HR (95% CI): 18.0 (5.64-57.3), 19.5 (2.07-184.9); preoperative adjusted OR (95% CI): 1.83 (1.19-2.81) and 5.04 (2.63-9.64), 9.83 (1.30-74.5); preoperative adjusted HR (95% CI): 2.90 (1.05-8.06), 6.53 (1.58-27.0), 7.52 (3.97-14.3); early postoperative OR: 19.6 (2.07-184.9), 1.12 (1.04-1.22); early postoperative adjusted OR: 1.12 (1.03-1.21)]. Statistically significant effects for other biomarkers were also reported in individual or a small number of studies (Table 1). Continuous and data-driven thresholds (ie. Youden index, ROC curve, quartiles) rather than pre-existing thresholds, were most commonly used and were inconsistent across studies. The majority of the studies were judged to have moderate to high risk of bias. A meta-analysis was initially intended, but significant heterogeneity of the data prevented the ability to perform a formal meta-analysis.
In summary, current literature included a number of biomarkers for prediction of VTE in cancer patients perioperatively and during hospitalization. However, data were severely limited due to the lack of descriptions for method of measurement, consistent thresholds and prospective data. Out of the biomarkers investigated, D-dimer showed promising results in predicting VTE incidence in perioperative and hospitalized cancer patients. Future prospective or interventional studies, involving a priori or continuous thresholds are needed to strengthen the use of candidate biomarkers in the prediction of VTE in perioperative and hospitalized cancer patients.
Disclosures
Wang:Valeo: Other: Advisory board; Servier: Other: Advisory board; Leo Pharma: Research Funding. Wells:Bayer HealthCare: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal